The Sovereignty of Disease
The Sovereignty of Disease

GENEVA: Information about infectious disease outbreaks travels today at speeds and in ways not imagined just 30 years ago. Individual countries can no longer ignore the disease or hide reports.
Enlarged image
In many instances the detection and response to the SARS outbreak appeared to infringe on national sovereignty, challenging the pre-existing norms that countries have the exclusive right to control the information they communicate and the public health measures they apply.
Despite widespread social disruption and economic loss, countries willingly collaborated in these measures of global solidarity. International travel to affected areas fell by 50 to 70 percent, hotel occupancy dropped by more than 60 percent, and businesses in tourism-related areas failed. Bio Economic Associates of Massachusetts estimates the direct and indirect costs of the outbreak at nearly US $100 billion.
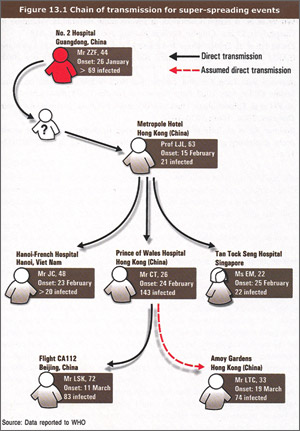
The book “SARS, How a Global Epidemic Was Stopped” describes these events that led to stopping the epidemic. It traces the SARS epidemic from its origins in the Guangdong Province of China to its international spread from a hotel in Hong Kong where a doctor infected in the Guangdong Province stayed overnight and inadvertently infected persons who carried the virus to neighboring Asian countries and as far away as Canada. It likewise details the epidemiology, natural history, and clinical signs and symptoms associated with human infection using easy-to-understand terminologies that make the book useful for health workers at all levels of the health system and of interest to the general public. Through personal stories and accounts of the outbreak, the book follows the epidemic from the initial description of an unknown respiratory disease in Vietnam by Carlo Urbani, a public health hero who himself became infected and died, to the last known cases of infection related to laboratory accidents in Singapore and China.
Chapters describe meetings at the highest political level, such as a meeting of the WHO regional director in the Western Pacific Regional Office and the former minister of health of China in late March 2003 to urge more transparent information-sharing; the infection’s impact on hospitals’ ability to maintain working conditions as health workers became infected; and elaborate measures taken by some countries to screen international travelers or quarantine those who had been exposed to infection. The book analyzes sites such as the Amoy Gardens Complex in Hong Kong, where 329 residents appear to have been infected by a series of events that led to environmental contamination of their bathing areas, and events such as Flight CA 112 from Hong Kong to Beijing, where at least 22 passengers and 2 crew members were infected by a passenger with signs and symptoms of SARS – explaining the role in amplifying transmission of the SARS Co-Virus. Illustrations show the individual chains of transmission from persons who carried infection to countries such as the Philippines, Mongolia and Vietnam.
In late 2003, another infectious agent that had first been shown to cross the species barrier between animals and humans in 1997 – the avian influenza virus (H5N1) – began spreading rapidly in poultry throughout Asia.
The recent international spread of another infectious disease, polio, has likewise demonstrated solidarity among countries. Since 2003, the wild poliovirus has spread to 25 previously polio-free countries, and these countries have freely exchanged genetic information about these viruses through the global polio surveillance network, linking each imported virus to its country of origin. The shared information has shown that northern Nigeria and northern India are the source of the virus in these re-infected countries, and neither country attempted to deny this fact.
SARS, polio and the H5N1 will not be the last new infections that flourish amid the conditions in a globalized world. Unlike SARS, emerging infections do not always transmit so easily from human to human. Some will emerge, cause illness in humans and then disappear, perhaps to recur at some time in the future. Others will emerge, cause human illness and transmit for a few generations, become attenuated, and likewise disappear. And still others will emerge, adapt to human populations and become pandemic or endemic, and remain intrinsic parts of our human infectious disease ecology. “SARS, How a Global Epidemic Was Stopped” shows how our globalized world set new norms and standards in infectious disease reporting and response, and provides many of the lessons needed to face these future public health assaults.
Click here to read an excerpt from “SARS: How a Global Epidemic Was Stopped.”
1 Heymann DL, Rodier G. Hot Spots in a Wired World. WHO Surveillance of Emerging and Re-emerging Infectious Diseases. "Lancet," 5 December 2001, 1: 345-353.
2 Heymann DL, Rodier G. Global Surveillance, National Surveillance and SARS. "Emerging Infectious Diseases," 2004, 10 (2): 173-175.
3 Heymann DL, Rodier G. SARS: A Global Response to an International Threat. "The Brown Journal of World Affairs," Winter/Spring 2004, X (2): 185-197.
4 Fidler DP. "SARS, Governance and the Globalization of Diseases." Plagrave Macmillan, 2004:50-60.
5 World Health Organization. "Situation Updates - Avian influenza." Available at: http://www.who.int/csr/don/archive/disease/influenza/en.
6 Global Polio Eradication Initiative. Global Case Count. At: http://www.polioeradication.org/casecount.asp.
7 World Health Organization. "Outbreak Associated With Streptococcus suis in Pigs in China: Update." At: http://www.wpro.who.int/media_centre/news/news_20050816.htm.
Dr. David L. Heymann is director of the Communicable Diseases Program at the World Health Organization.