Seeking Access to Life-Saving Vaccines
Seeking Access to Life-Saving Vaccines

NEW HAVEN: The humanitarian organization Médecins Sans Frontières has begun vaccinating refugee children in Greece against a leading cause of pneumonia that remains the single largest killer of children worldwide. Each year, pneumonia contributes to an estimated 1 million child deaths.
Médecins Sans Frontières can access the pneumonia vaccine at reduced prices through a mechanism available for use in humanitarian settings, recently negotiated by that group along with the World Health Organization, Unicef and Save the Children, that enabled a purchase price at a rate of US$9 per child. However, the vaccine is among a handful of newer vaccines, developed within the last 20 years and recommended by the World Health Organization, which remain unaffordable for many families around the world.
Recent outbreaks of measles throughout the world have prompted alarm among public health officials and the public about the growing phenomenon of vaccine refusal and hesitancy. The campaign in Greece highlights another critical part of the story – many children miss out on potentially life-saving vaccinations because they are costly and not readily available.
About 35 percent of the world's children – more than 55 million children – live in countries that do not routinely vaccinate children against pneumonia. A key barrier for countries considering the vaccine is cost. The pneumococcal conjugate vaccine, first developed in 2001, is among the most expensive vaccines recommended for children. The technological advance of “conjugation” allows for the vaccine to be used in children under one year of age, unlike its predecessor the pneumococcal polysaccharide vaccine. Up until recently, just two pharmaceutical companies – Pfizer and GlaxoSmithKline – produced the vaccine, and limited competition provided little incentive to reduce prices. In the United States, the vaccine is priced at $137.01 for Centers for Disease Control vaccine contracts and $180.05 on the private market. Despite no changes in the composition, prices for this vaccine in the United States have increased about 5 to 8 percent annually between 2010 and 2017.
Pneumonia, an infection of the lungs, is a disease linked to poverty. Therefore, the pneumococcal vaccine, which could prevent up to a half of severe cases, is particularly critical for this at-risk group. Illness can progress quickly – a child who has a mild cough in the morning can be gravely ill and struggling to breathe by evening. Factors such as air pollution, household crowding and malnutrition increase children’s risk of developing the disease. Problems accessing or affording healthcare and timely treatment result in children dying of pneumonia. While many children across the world contract pneumonia, the majority of deaths occur in low- and middle-income countries.
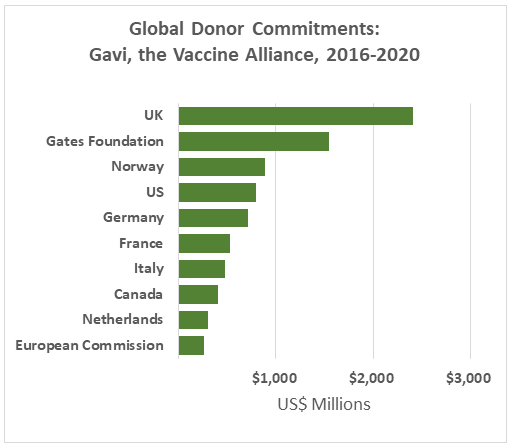
Low-income countries can access the pneumonia vaccine at lower costs through Gavi, the Vaccine Alliance – a donor-funded organization that supports vaccine implementation. Gavi was created in 2000, through an initial grant by the Bill and Melinda Gates Foundation, to help close the “vaccine gap” between the adoption of newly developed vaccines in high-income countries compared to low-income countries. It provides support to more than 50 countries whose gross national income per capita has been less than or equal to US$1,580 over the past three years.
Therefore, the main squeeze for affording the vaccine occurs in middle-income countries, such as China, and many have yet to introduce the vaccine. Furthermore, there are 20 countries, including India, Nicaragua and Nigeria, set to lose their eligibility for Gavi support by 2020 as their gross national income per capita exceeds the set threshold. Many emerging economies will find it challenging to afford existing vaccine programs. And although Gavi also pays the $9 price available to humanitarian organizations, the vaccine remains among the most expensive in Gavi’s toolkit, accounting for 40 percent of its entire vaccine budget. Lowering vaccine costs would enable Gavi to stretch its budget to accommodate other programs.
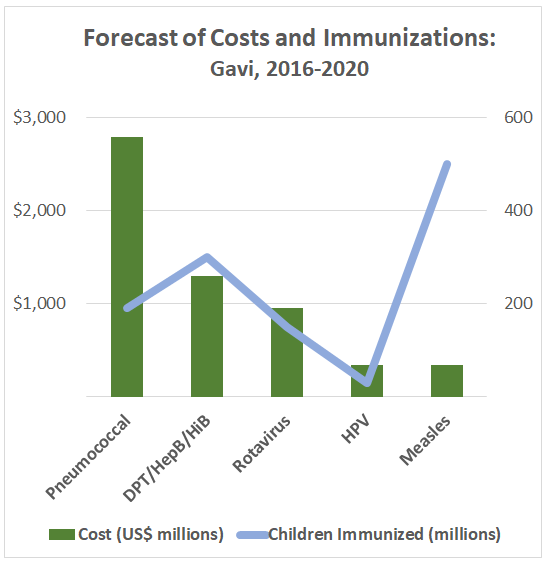
While Gavi has helped more than100 million children in low-income countries access the pneumococcal vaccine, it has so far struggled in another objective – bringing down the price of the pneumococcal vaccine. The US$1.5 billion “Advanced Market Commitment,” funded by Canada, Italy, Norway, Russia, the UK and the Gates Foundation, guaranteed a market for the vaccine at a fixed price. The plan was supposed to incentivize pharmaceutical suppliers in low-income countries to produce the vaccine, thereby increasing competition and reducing prices.
A major challenge for manufacturers interested in developing more affordable versions of the vaccine are the many patents, which can cover all aspects of vaccine development including starting materials, procedures for manufacturing the vaccine and administration. By taking out patents on incremental improvements for the vaccine, a process known as “evergreening,” pharmaceutical companies can extend their patents on existing products. Indeed, Médecins Sans Frontières is currently challenging patents for the pneumococcal vaccine, which is nearly 20 years old, in India and South Korea – countries well-positioned to produce quality and affordable vaccines, in an effort to increase global competition.
Despite these challenges, a third manufacturer from India is about to enter the market with a lower price alternative, estimated at $6 per child. The Serum Institute of India has applied for WHO pre-qualification - a quality and safety approval, and Executive Director Suresh Jadhav expects that approval process to be complete by the end of the year.
Researchers, concerned about the vaccine’s cost and accessibility, are exploring whether health providers can safely reduce the number of doses given to infants, from the current standard of three for infants, without losing the protection that it provides. This strategy has just been introduced in the United Kingdom, and studies are underway in Vietnam, India, South Africa and Gambia to determine whether this approach works in low and middle-income countries, where children are more at risk of pneumonia.
Even in countries where the pneumonia vaccine is freely available, there continue to be issues with vaccine access. In the United States, the pneumonia vaccine is freely available for all children under the Vaccines for Children program, however coverage rates for most vaccines are lower among uninsured children and children living in rural areas. Issues such as unfamiliarity with the program and access, transportation, childcare and proximity, especially in rural areas, may be to blame.
As a global community, we have a responsibility to ensure that basic health interventions are reaching children who need it the most. This requires addressing access to vaccines, a far too common challenge, in addition to hesitancy.
Jocelyn Chan, 2018-2019 International Fox Fellow at Yale University, is a medical doctor and PhD Candidate at the University of Melbourne. Her current work addresses pneumonia, which is one of the leading causes of childhood mortality worldwide. She has worked as an epidemiologist with Médecins Sans Frontières in South Sudan and assisted in the Ebola outbreak response in Sierra Leone with the World Health Organization.