WHO Criteria for Lifting COVID-19 Restrictions
WHO Criteria for Lifting COVID-19 Restrictions
EAST LANSING: The goal for most countries is to restore economic activity as quickly as possible. Yet many leaders differ, continuing to provide mixed messages on reopening similar to how many rejected early warnings and the need to prepare. Availability of a vaccine is at least a year away, and to ensure safety and stop transmissions, the World Health Organization recommends that nations satisfy six criteria.
Transitioning to and Maintaining Steady State of Low-Level or No Transmission
1 COVID‑19 transmission is controlled to a level of sporadic cases and clusters of cases, all from known contacts or importations and the incidence of new cases should be maintained at a level that the health system can manage with substantial clinical care capacity in reserve.
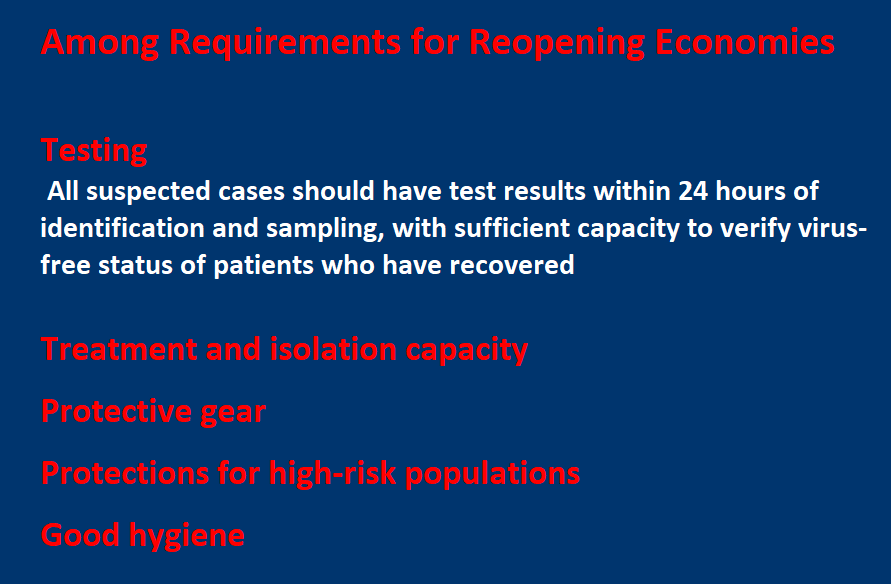
2 Sufficient health system and public health capacities are in place to enable the major shift from detecting and treating mainly serious cases to detecting and isolating all cases, irrespective of severity and origin:
• Detection: suspect cases should be detected quickly after symptom onset through active case finding, self-reporting, entry screening, and other approaches;
• Testing: all suspected cases should have test results within 24 hours of identification and sampling, and there would be sufficient capacity to verify the virus-free status of patients who have recovered;
• Isolation: all confirmed cases could be effectively isolated, in hospitals or designated housing for mild and moderate cases, or at home with sufficient support if designated housing is not available, immediately and until they are no longer infectious;
• Quarantine: all close contacts could be traced, quarantined and monitored for 14 days, whether in specialized accommodation or self-quarantine. Monitoring and support can be done through a combination of visits by community volunteers, phone calls, or messaging.
3 Outbreak risks in high-vulnerability settings are minimized, which requires all major drivers and/or amplifiers of COVID‑19 transmission to have been identified, with appropriate measures in place to minimize the risk of new outbreaks and of nosocomial transmission: for example, appropriate infection prevention and control, including triage, and provision of personal protective equipment in health care and residential care settings.
4 Workplace preventive measures are established to reduce risk, including the appropriate directives and capacities to promote and enable standard COVID-19 prevention measures in terms of physical distancing, hand washing, respiratory etiquette and, potentially, temperature monitoring.
5 Risk of imported cases managed through an analysis of the likely origin and routes of importations, and measures in place to rapidly detect and manage suspected cases among travelers, including the capacity to quarantine.
6 Communities are fully engaged and understand that the transition entails a major shift, from detecting and treating only serious cases to detecting and isolating all cases, that behavioral prevention measures must be maintained, and that all individuals have key roles in enabling and implementing new control measures.
Many nations continue to struggle to offer adequate testing and secure protective gear for health care providers. Any community with lax standards is a threat to the rest of the world. “The global response to the COVID-19 pandemic requires the capacity to conduct ongoing risk assessment at the global, regional, national, and subnational levels,” the report notes.
International cooperation centers on technical expertise: “Experts from around the world and frontline responders are reviewing all available evidence to develop and update technical guidance for countries to prepare and respond to COVID-19.” The United Nations has also organized a Supply Chain Task Force, to ensure strategic distribution of protective gear and other medical supplies.
Shortly after WHO announced its guidelines, US President Donald Trump announced suspension of US funding for the organization that is distributing test kits and advising governments around the globe, suggesting an investigation “to assess the World Health Organization’s role in severely mismanaging and covering-up the spread of the coronavirus.” He blamed WHO for relying on China’s disclosures. about the disease.
“America and the world have chosen to rely on the WHO for accurate, timely and independent information to make important public health recommendations and decisions.... our country will be forced to find other ways to work with other nations to achieve public health goals.... Those tasked with being truthful and transparent have failed to do so. It would have been so easy to be truthful.” He then went on to suggest that so much death is due to WHO mistakes.
WHO announced a global emergency on January 30, but many leaders, including Trump, disregarded the warning and did not rush to prepare with testing or building hospital capacity. The United States reports the world’s highest number of confirmed cases, more than 600,000 with more than 26,000 deaths.
Nations continue to give mixed messages on COVID-19 and economic consequences and reopening.
Accurate information is key to battling the pandemic, concludes WHO. “Unfortunately, the global public health response to the COVID-19 pandemic has been accompanied by an infodemic, which is an over-abundance of information – some accurate and some not – that makes it hard for people to find trustworthy sources and reliable guidance when they need it,” the report notes. “This misinformation hampers public health responses to epidemics and prevents people from taking adequate measures to effectively prevent disease transmission. Some misinformation may also lead to dangerous behaviours, such as self-medication with harmful substances.”
The report concludes with the hope that the world emerges with stronger health systems and improved global collaboration to counter future pandemics: “We must learn the lessons of this pandemic now and, in so doing, ensure that our response, wherever possible, leaves a lasting positive legacy, and makes the world of the future a safer place.”
Read the WHO’s COVID-19 Strategy Update.
Comments
How does WHO help poor countries or economies mainly in Sub Saharan Africa and Asia to adequately adhere and implement the guidelines? Tanzania, for instance, opted for other measures to contain the disease because it can't afford to take care of it's poverty stricken communities by implementing a total lockdown. In my opinion, I think you should treat such countries separately by considering their economies, health system capacity in terms of facilities and workforce on the ground.