The Deadliest Nations for Covid-19
The Deadliest Nations for Covid-19

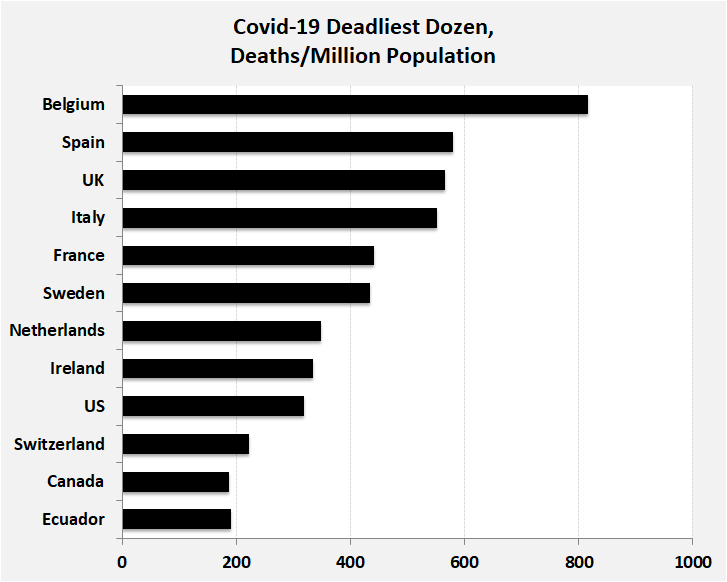
NEW YORK: Covid-19 presents many unknowns – and why the populations of 11 wealthy developed countries in Western Europe and North America experience the world’s deadliest mortality rates remains a mystery. In the absence of a widely available vaccine, resolving that mystery may prove instructive on deciding how best to address this pandemic and those likely to occur in the future.
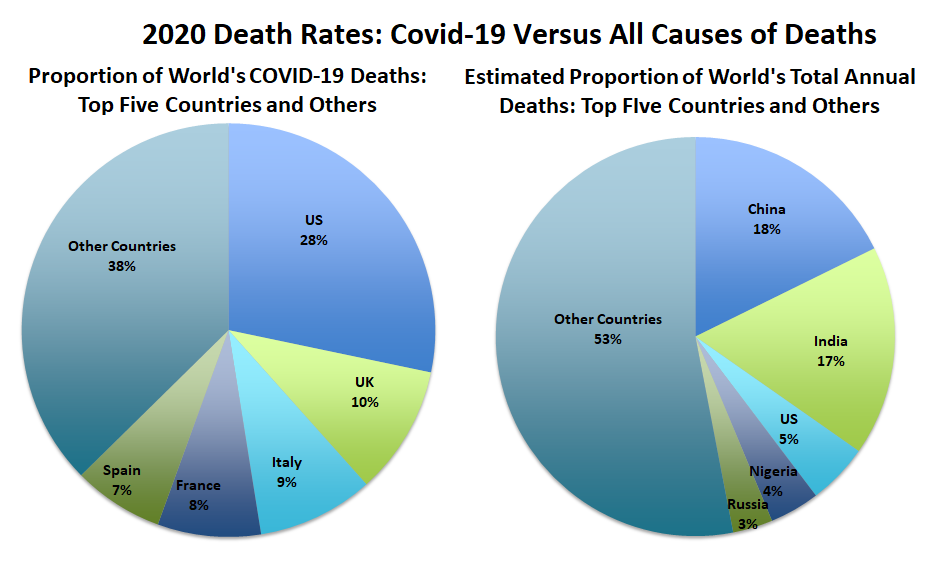
Just five countries account for nearly two-thirds of all Covid-19 deaths: the United States, followed by the United Kingdom, Italy, France and Spain. The coronavirus experience of the United States, particularly noteworthy, is worthy of in-depth analysis. The United States, representing 4 percent of the world’s population, accounts for 28 percent of global Covid-19 deaths and 29 percent of reported coronavirus cases. In striking contrast, China and India, each representing 18 percent of the world’s population, account, for 1 percent each of all Covid-19 deaths worldwide and 1 percent and 3 percent, respectively, of reported cases.
An initial explanation for the large differentials in Covid-19 mortality rates among countries emphasized differences in sampling and national reporting. Some public-health analysts initially suspected that many governments underreported and undercounted deaths.
Some governments may have deliberately underreported Covid-19 deaths for political reasons. For example, while its neighbors report thousands of coronavirus infections and hundreds of resulting deaths, North Korea reports zero cases. In Belarus, the country’s president declared at the end of April that his country had no confirmed cases and, unlike neighboring governments, imposed no restrictions on the population. By the end of May, Belarus reported about 43,000 confirmed cases and 235 deaths.
In other countries, undercounting of Covid-19 deaths was largely a combination of misdiagnosis, testing shortages and shortcomings in the collection and reporting of vital statistics. Most countries, with Belgium the notable exception, report only those Covid-19 deaths that take place in hospitals or when a test confirms coronavirus infection. One analysis of 25 countries covering recent months found at least 87,000 more people died during the coronavirus pandemic than the official Covid-19 death counts report. In many countries, including the United States, Indonesia and Mexico, deaths and burials proceed with no testing of the deceased to determine infection.
Most observers conclude that Covid-19 deaths have indeed been underreported. However, comparative analyses of available data suggest that this is an unlikely explanation for the deadliest Covid-19 rates.
Surprisingly, in contrast to their high Covid-19 death rates, the top 11 countries have achieved comparatively low overall mortality rates. Life expectancies at birth are about 10 years higher than those of less developed countries and nearly 5 years higher at age 60.
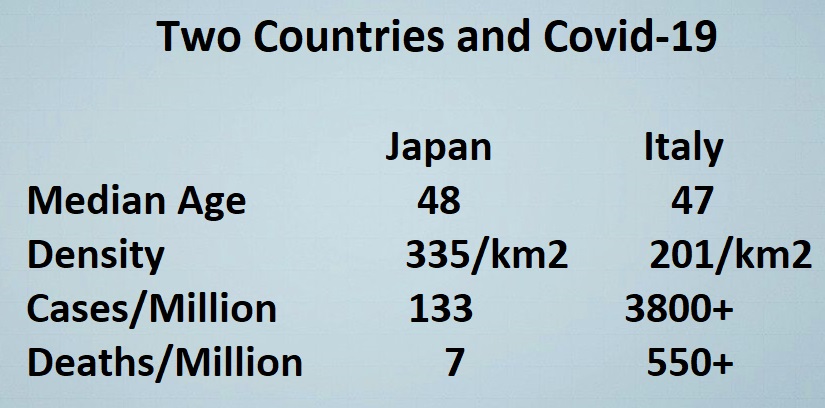
Covid-19 deaths are heavily concentrated among the elderly, especially those in long-term care facilities. In the United States and Sweden, for example, those over age 65 account for no less than 80 percent of the coronavirus deaths. With this in mind, public health analysts initially theorized that comparatively older age structures of countries offered an explanation. Reported data, however, are not consistent with that explanation. A simple comparison of Italy and Japan, two countries with similar age structures and high life expectancies, finds Italy’s Covid-19 death rate close to 80 times greater than Japan’s, 551 versus 7 deaths per million, respectively.
Another proposed explanation for deadliest Covid-19 rates targeted high levels of population density and urbanization. Again, available data do not support that proposition.
Countries with similar or higher population densities, such as Israel, Japan, Republic of Korea and Singapore, have substantially lower Covid-19 death rates than the countries with the deadliest rates. Similarly, while New York, Paris and London are devastated, other large metropolitan areas such as Bangkok, Baghdad, New Delhi and Lagos are substantially less affected.
Comparisons among neighboring countries with similar climate conditions also provide little insight to explain differences in Covid-19 death rates. Germany’s death rate, for example, is about a quarter of the rate of France and the Netherlands. The death rate in Iran is nearly 20 times larger than Iraq’s rate, 93 versus 5 per million population.
Lockdowns, social-distancing, facemasks, tracing contacts, case isolation and related measures have reportedly been effective in reducing Covid-19 death rates in many countries. However, some countries that avoided nationwide lockdowns and social-distancing requirements, such as Myanmar and Cambodia, report comparatively low death rates. One possible explanation is that the coronavirus arrived in those places at a later date and death rates may still rise.
In addition, several European countries, such as Sweden and to a lesser extent the Netherlands, perhaps aiming to achieve “herd immunity,” minimized restrictions, banning gatherings of 50 or more, yet permitting restaurants and bars to remain open while relying on citizens to self-regulate. To date, those countries have achieved lower Covid-19 death rates than countries with more stringent lockdowns and social-distancing measures, such as Belgium, Italy and Spain.
In addition, Sweden reports that by the beginning of May more than a quarter of the 2 million people residing in the country’s capital, Stockholm, had been infected by the coronavirus. The Swedes and the Dutch argue that their decisions on how to deal with the coronavirus pandemic are preferable to the policies of nearby European countries whose governments now struggle on how to maintain safety while reducing restrictions, transition from lockdowns and restart depressed economies.
The experiences of Denmark, Finland and Norway suggest that early lockdowns may have prevented excess deaths. Those three Scandinavian countries announced nationwide lockdowns in early March before registering any coronavirus deaths. Consequently, at the end of May their numbers of coronavirus deaths per million were a fraction of the comparatively high death rates in Sweden and the Netherlands.
Public health experts propose various explanations for the enormous differences in Covid-19 death rates. Virtually all of them come with cautions, provisos and puzzling counterevidence that undermine their soundness. Cursory analysis suggests there may be no simple, single explanation for why the populations of wealthy developed countries in Western Europe and North America experience the world’s highest Covid-19 mortality rates. Instead, the answer to that mystery is likely a complex combination of critical factors, with the most prominent as follows:
Demographics, including age structure, density, urbanization, mobility, migration, morbidity and health;
Environment, including location, climate, temperature and sunshine;
Culture, including social distance, contacts, physical interactions such as handshakes and hugs, nutrition and obesity rates, and hygiene;
Society, solidarity, cooperation, responsibility and adaptability;
Government, speed/type of responses, unified messaging, leadership, credibility, prevention and healthcare systems.
In addition to the enormous country differences in Covid-19 death rates, the numbers of deaths, approaching 400,000, continue to mount daily as the disease spreads around the planet. In the absence of a worldwide available vaccine, for which many countries race to discover, a significant proportion of world population could become infected – up to 70 percent to achieve herd immunity, which is unlikely to be achieved any time soon – and more than 50 million could succumb to Covid-19.
Unfortunately, the worst of the pandemic may be ahead. Most countries are relaxing policies of lockdowns and social isolation, understandably trying to revitalize depressed economies and return to normal lifestyles. Without use of social distancing, facemasks and other safeguards, however, public health experts anticipate a resurgence later this year, as was tragically experienced in the deadly 1918 influenza pandemic.
Without question, Covid-19 is exacting heavy demographic, social and economic tolls worldwide. Perhaps the only consolation emerging from the current pandemic is that it has made the world’s population of men, women and children considerably more cognizant and sensitive to the value of good health, the precariousness of human life, the essentiality of social and communal interactions, the capriciousness of death, and the interconnectedness of humanity.
Joseph Chamie is an independent consulting demographer and a former director of the United Nations Population Division.
This article was posted June 1, 2020.
Comments
The high mortality rates bcs these countries caused considerable pain and suffering during the centuries of colonial conquests and war mongerings. Is karma at its best. There is a God afterall.
Dear Mr. Chamie,
At least one factor has been overlooked
The financial factor.
But the self-interest factor must not be overlooked either
I am an economist and do not support any conspiration theory, so don't get me wrong.
For a person's real motivation in decision making I look at their actions and try to ignore their published motivations. Or as proverbial judge Rice from around New Orleans sais “There are two reasons for every action. The good reason, and The real reason”
My oldest brother was a medical doctor in the Netherlands. From him I learned that the official but unpublished guideline for doctors was that people above 70 to 75 years old were supposed to have had a fulfilled life and should only give medicines to keep them more comfortable, but not medicines to prolong their life. After all he added every older person is drawing a pension and the longer they live the costlier it becomes. He died accordingly when he got a deadly cancer at 73. When I asked him why he was not doing everything he could to get the urgent operation he needed to live a few more years, heanswered that that was not according to the guidelines he had followed.
So look at the financial factor in every country to see who benefits most. In nations like The Netherlands, Sweden and others where most of those who died were people over 60 and the country had a strong financial support system for those the hidden attitude may not have been to really save older victims but to reduce suffering.
For the self interest factor we must look at who the victims are and which motive could have played.
In one country the victims are more likely to come from the party that mostly relies on the support from the less wealthy (the poor) If the political party in power relies on the support of the wealthier part of the nation there could be a tendency to slack in measures that prevent the spread of the virus.
In at least one such country that is what we see in practice. This in spite of loudly proclaiming the opposite from time to time. Draw your own conclusions but never ever forget that money and self-interest have the largest influence on any decision by politician and business people.